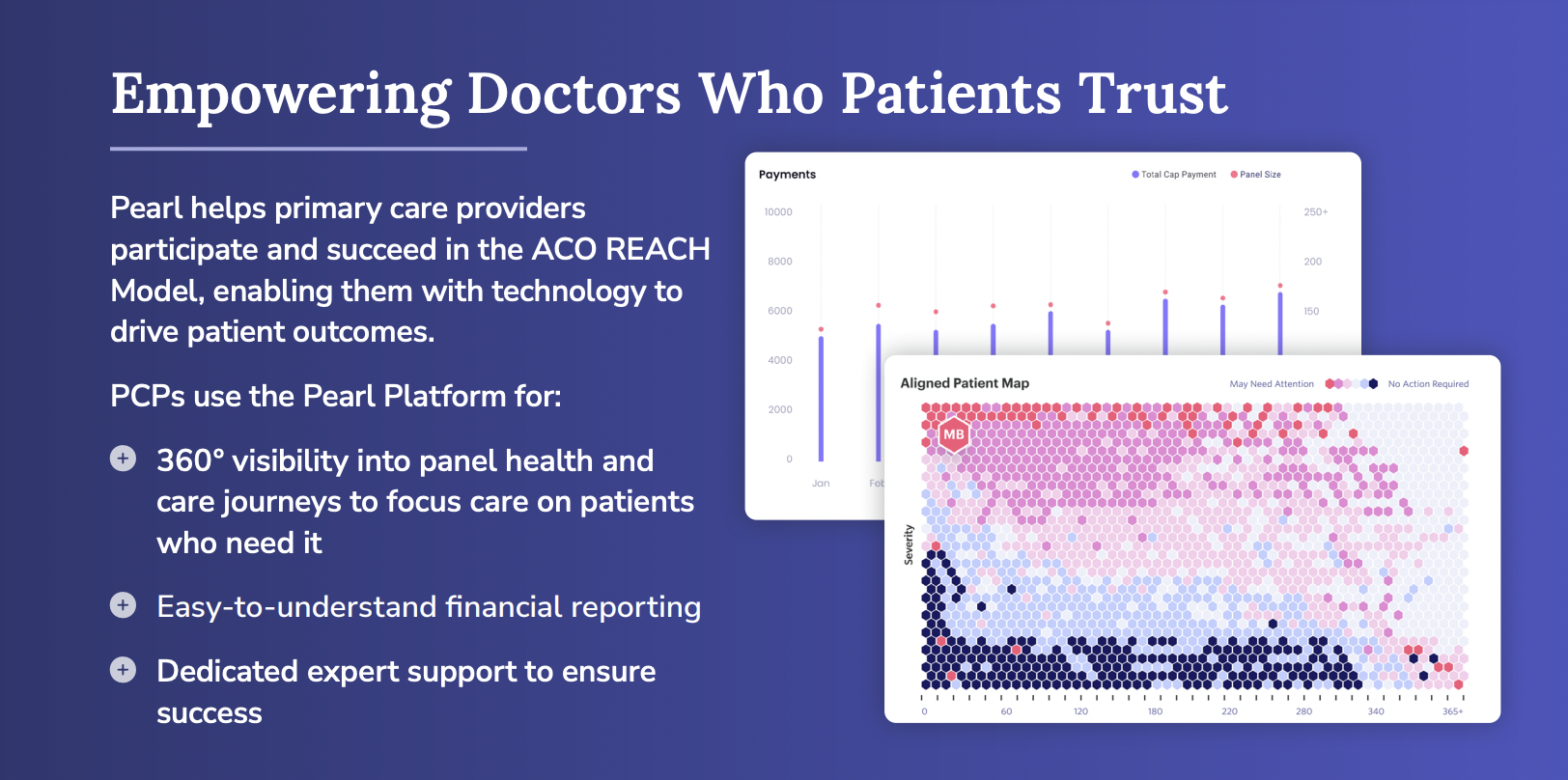
The Accountable Care Organization Realizing Equity, Access, and Community Health ACO REACH Model (formerly known as Direct Contracting) is an alternative payment model launched in 2020 — and renamed in February 2022 — by the Centers for Medicare and Medicaid (CMS) to encourage primary care physicians (PCPs) and other eligible professionals to shift away from fee-for-service (FFS) compensation to valuebased payments in primary care. ACO REACH helps empower PCPs with autonomy to deliver care as they see fit by realigning financial incentives with patient outcomes, not volume.
What is ACO REACH?
WHAT YOU NEED TO KNOW
• ACO REACH gives PCPs revenue stability and predictable cash flow with stable monthly payments for aligned Medicare patients, instead of the volatility of FFS.
• ACO REACH gives PCPs the opportunity to bear and capture value from risk, generating shared savings from quality care that is managed and delivered at a lower cost.
• ACO REACH beneficiaries are still enrolled in Original Medicare with the same rights and benefits, like the MSSP ACO program but without the baggage
ACO REACH — Financial Impact
Aligning incentives with value created for Medicare patients Although many primary care providers (PCPs) invest significant amounts of their time and resources in community-based care management and coordination for their patients — including underserved communities — it’s insurers who are most likely to profit from the value their work creates. Medicare’s Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) Model provides an opportunity for PCPs to capture the full dollar value generated from effectively managing care for Medicare patients. PCPs can use these funds to reinvest in their staff, their practices, and their patients.
ACO REACH provides an alternative payment model with two key features:
- Capitation: stable monthly payments for every Medicare patient to whom you provide primary care services.
- Shared Savings: annual payments for savings from managing the Total Cost of Care for Medicare patients lower than a benchmark. Additional (i.e., non-primary care) procedures continue to be paid on a fee-for-service (FFS) basis, reducing sharp negative income changes.